Learning Beyond the Classroom
MY STORYEntering the community as a learner
Listening to residents’ experiences forced me to reconsider my initial assumptions. Individuals often labeled as “difficult to engage” were not disengaged by choice, but were responding to long histories of stigma and instability that standardized interventions cannot address.
When access did not mean preparedness
What I initially understood as an individual burden soon exposed structural gaps that reshaped how I approached overdose prevention. After an assessment with an older resident, I asked whether she needed naloxone. She told me she did not, because it was given freely through DESC, but then told me with striking seriousness that people were not dying because they lacked naloxone. They were dying because no one had taught them how to use it. Her friends overdosed while holding naloxone, unsure how to administer it. When she was not present, more people died despite having access.
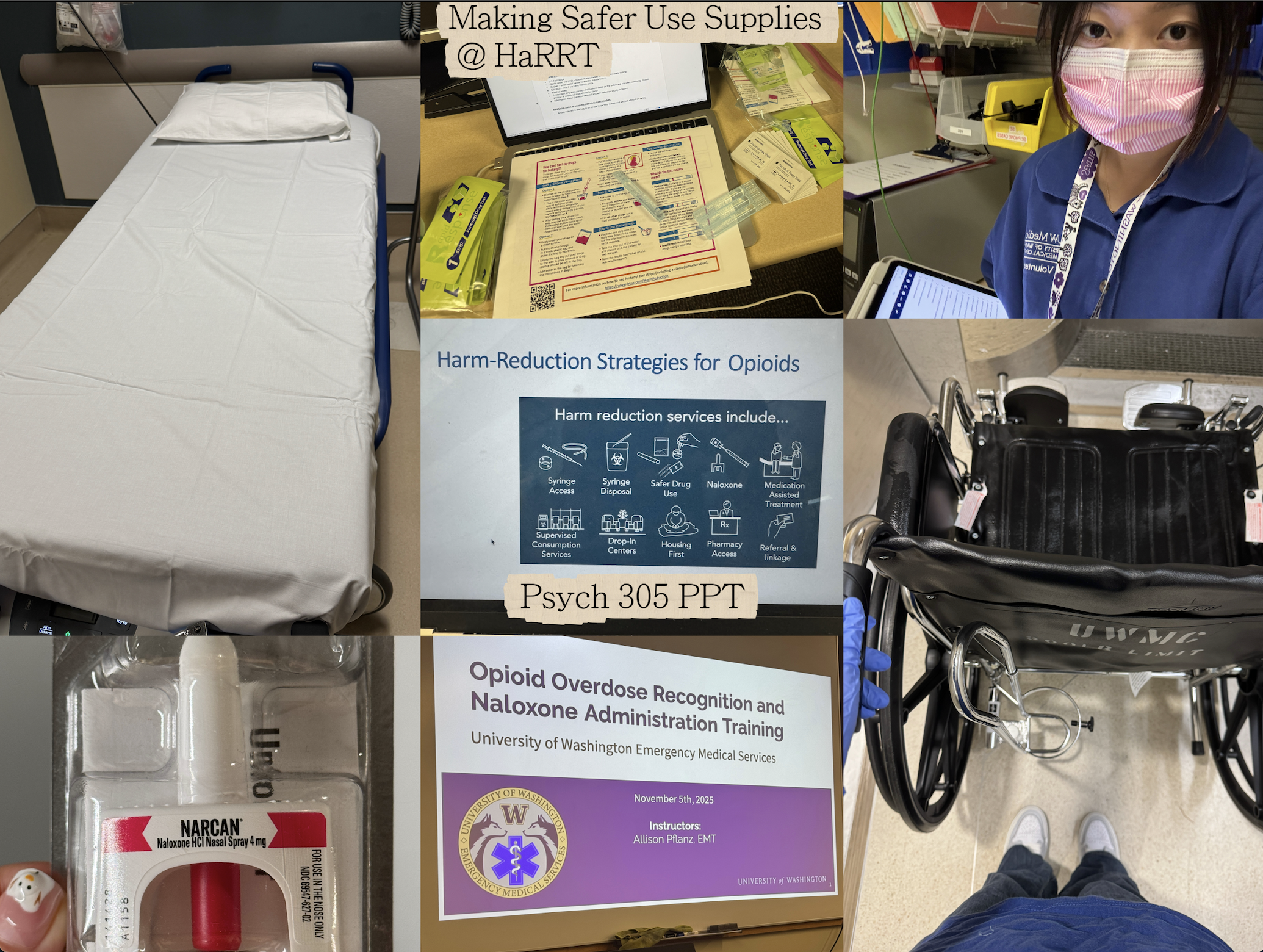
When I returned to the lab, I shared this experience with my principal investigator, and then our team created instructional materials alongside harm reduction supplies to address this gap. I also completed naloxone administration training, so that, if an emergency arose, I would be prepared to help.
Care at the margins of the healthcare system
I encountered a different expression of these same structural gaps while volunteering in the emergency department. Patients often arrived with not only medical concerns, but also fear shaped by language barriers, stigma, and unfamiliarity with the healthcare system. Some apologized repeatedly for asking questions, unsure whether they were allowed to seek clarification. Being present in these moments, I offered reassurance, explained procedures, and stayed alongside patients during uncertainty, which showed me how quickly discomfort escalates when people feel unseen.
Seeing this in the emergency department made what I had learned about health disparities feel real, as I watched how trust, communication, and feeling safe enough to ask questions shaped people’s care.
How the community reshaped my practice
All experiences changed how I approach research and care, grounding my work in listening, trust, and accountability to the communities involved. Now, I see engagement not as a step in a project, but as an ongoing responsibility shaped by the people I work alongside.
My most formative learning at the University of Washington occurred through community-engaged work with the Harm Reduction Research and Treatment (HaRRT) Center in permanent supportive housing.
I supported consent procedures and assessments for a digital harm reduction intervention with residents experiencing chronic instability. Through these interactions, I learned about the depth of loneliness shaped by stigma and long-standing disconnection from systems intended to provide support.